The 100-year search for an alternative heart

Bettmann // Getty Images
The 100-year search for an alternative heart
About 2,000 hearts are available each year for transplantation, but more than 3,000 people are on the heart transplant list. A 2021 study published in the Journal of the American Heart Association found that over the past decade, the percentage of organs accepted for transplant has not increased proportionally to the number of donor hearts offered for transplant.
The challenge of finding a donor heart has long motivated scientists to develop an artificial heart. Their goal is to provide artificial hearts as a temporary option so that patients who would not otherwise survive on a temporary pump have more time until a donor heart can be found.
In 2008, surgeons at Johns Hopkins Medicine recommended that for a hospital to be named a high-volume facility, it should perform 14 procedures a year—an increase from the earlier benchmark of 10 procedures a year. Patients who receive their transplants at high-volume facilities have a better survival rate and fewer complications.
“The bar for patient safety, quality of care, and survival needs to be set pretty high,” said senior study investigator and cardiac surgeon John Conte. The U.S. health care system must rethink which hospitals should do heart transplants.
Citing studies from Cardiology Research and other scientific publications, Healthmatch compiled a timeline of the development of an alternative human heart.
![]()
Pictorial Parade/Archive Photos // Getty Images
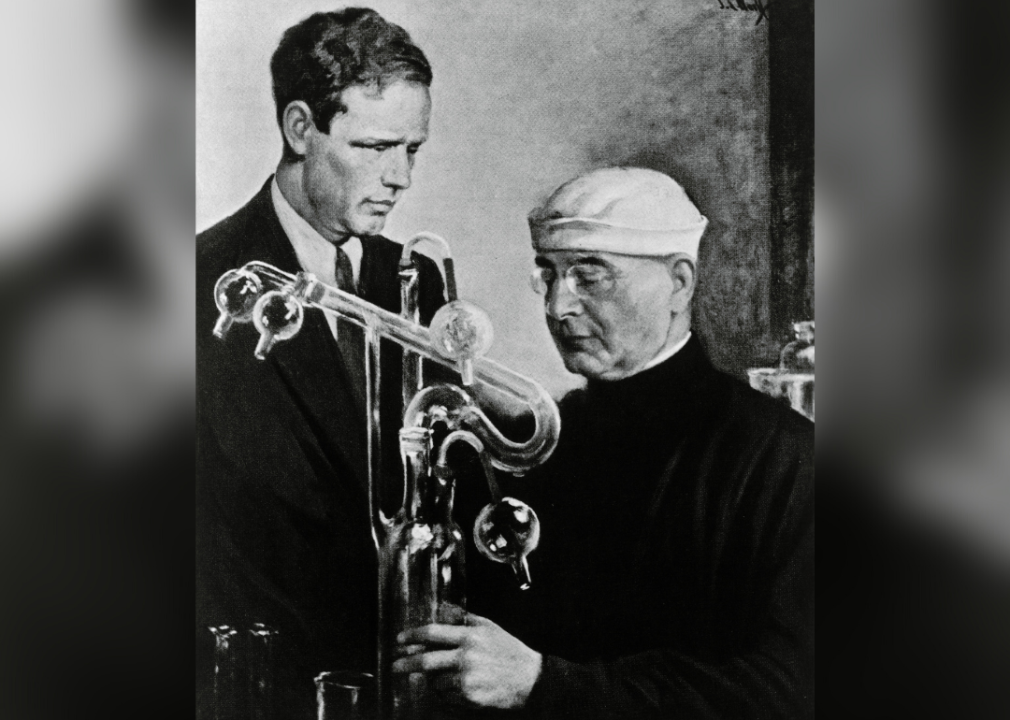
1920s: First hearts are kept alive outside of the human body
In the 1920s, aviator and inventor Charles Lindburgh and surgeon Alexis Carrel collaborated to develop an external blood pump for use during heart surgery. After a few failed attempts, Lindbergh created a pump that worked. He and Carrel subsequently developed an in vitro “artificial heart-like” device to keep organs alive outside the body. They removed hearts, kidneys, ovaries, and thyroid glands, and used their invention to monitor the development and function of these organs.

Keystone-France/Gamma-Rapho via Getty Images
1937: First artificial heart implanted in dog
In 1937, Russian scientist Vladimir Demikhov, developed a device called a total artificial heart. The device comprised two side-by-side pumps powered by an external motor with a transcutaneous drive shaft inserted through the skin. The device was transplanted into a dog, which lived for five-and-a-half hours after the operation.
AFP via Getty Images
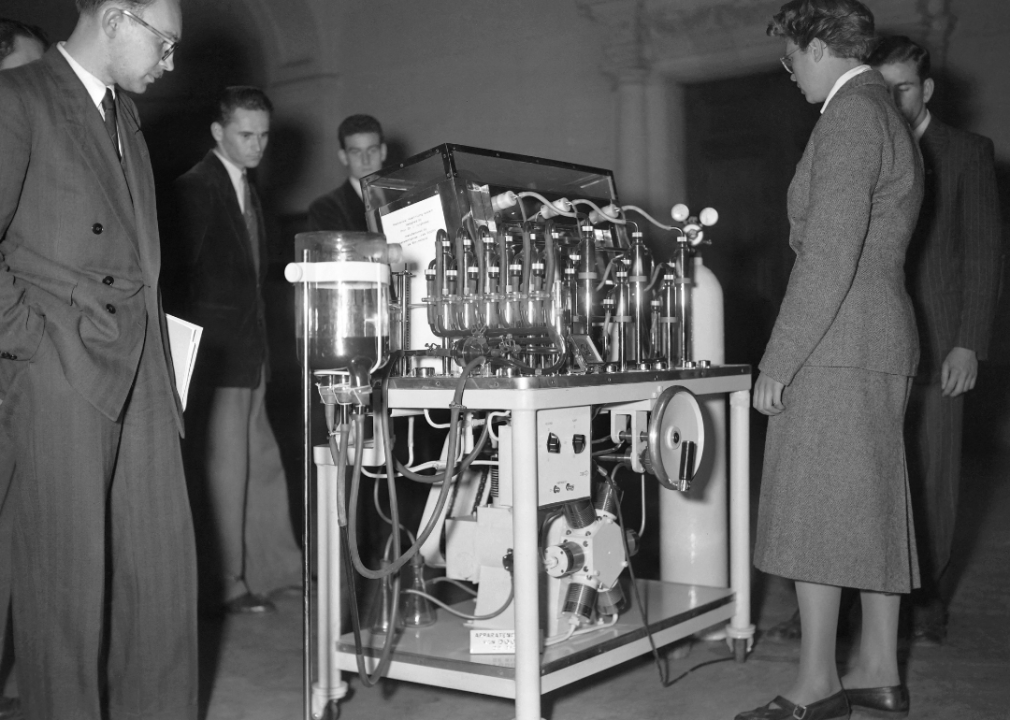
1953: Heart-lung machine is used to perform first successful cardiopulmonary bypass
In 1953, Dr. John Gibbon Jr., a surgeon at Jefferson Medical College, saw the culmination of 20 years of work when he successfully performed heart surgery on 18-year-old Cecelia Bavolek. In 1931, Gibbon began developing an external heart-lung machine following the death of a patient during surgery. After years of animal experiments, the machine was ready for use in humans. Bavolek’s heart was connected to the machine for about 45 minutes while Gibbon repaired a heart defect. She recovered fully from the operation.

FPG // Getty Images
1963: Paul Winchell patents first artificial heart for humans
Paul Winchell, a voice-over actor and ventriloquist, claimed to be the first person to patent an artificial heart. He claimed Dr. Robert Jarvik copied his idea to develop what came to be known as the Jarvik-7 artificial heart. However, patents for an artificial heart had been filed before Winchell’s invention.
Winchell collaborated with surgeons at the University of Utah to develop his device. A nontoxic bag implanted in the body was powered by a battery-operated motor worn outside the body to simulate the pumping action of a real heart. Winchell hoped his invention would replace a failing heart. Unfortunately, the device, as developed by Winchell, was unable to sustain human life for any significant period of time.

Bettmann // Getty Images
1964: Artificial Heart Program created by National Institutes of Health
The goal of the Artificial Heart Program, a multimillion-dollar initiative, was to develop an artificial heart that could be implanted in humans by the end of the decade. Teams of engineers were awarded grants in a competition to develop the best pump, valve, or power source. A few teams even experimented with nuclear-powered hearts, albeit unsuccessfully. The project was featured on the covers of Time and Life magazines.

Christopher Furlong // Getty Images
1964: First human-chimpanzee heart transplant
Impressed by Dr. Keith Reemtsma’s work transplanting chimpanzee kidneys into human recipients, Dr. James Hardy, a surgeon, was determined to perform the first clinical heart transplant. Hardy transplanted a chimpanzee heart into a patient whose severe atherosclerotic cardiovascular disease had necessitated the amputation of both legs. Unfortunately, the chimpanzee heart was not large enough to sustain adequate circulation and failed a short time later. The public and medical community had a very negative response to news of the procedure, so Hardy and his team decided not to attempt another chimpanzee-to-human heart transplant.
Keystone/Hulton Archive // Getty Images
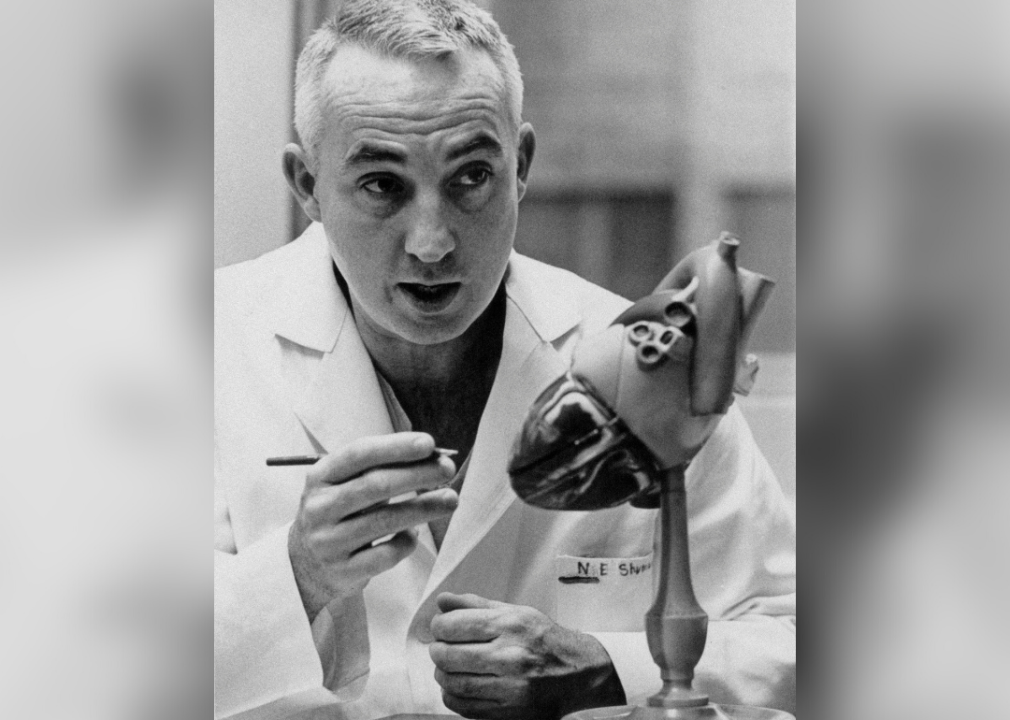
1966–69: First artificial hearts implanted in patients
In 1966, Dr. Michael DeBakey, a cardiovascular surgeon at Houston Methodist Hospital, implanted a partial artificial heart into a patient. This breakthrough was followed by the first successful human heart transplant in 1967 by Dr. Christiaan Bernard, a South African surgeon. At the Texas Heart Institute in 1969, Dr. Denton Cooley successfully transplanted the first artificial heart into a human patient. The patient received a human donor heart three days later but died one-and-a-half days after that.
Bettmann // Getty Images
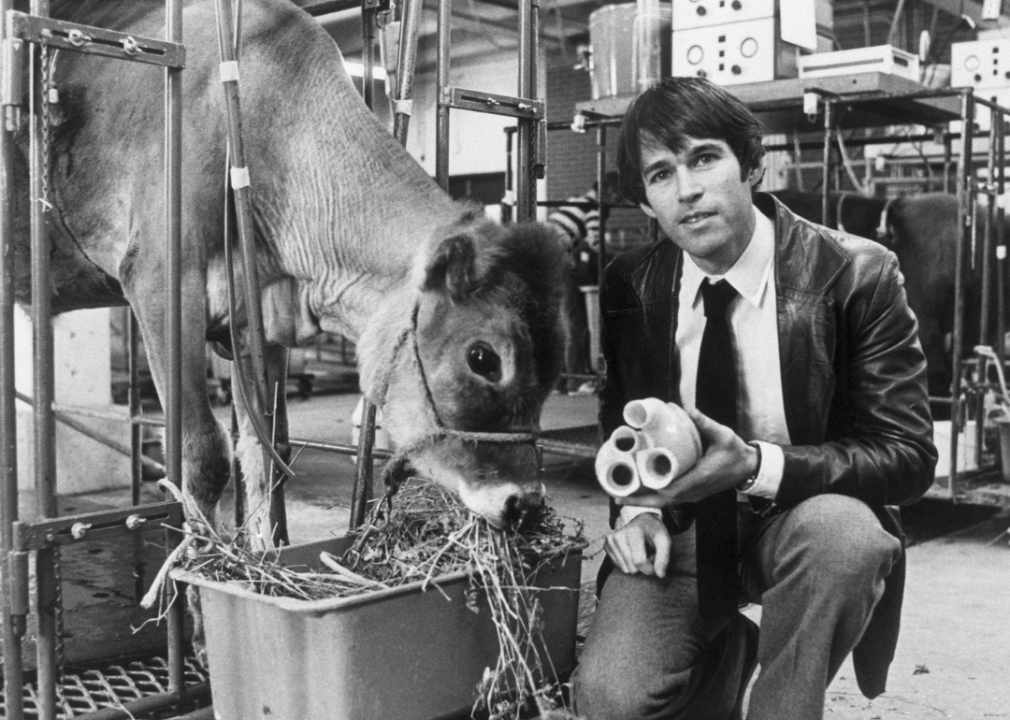
1982–85: Jarvik-7 heart raises ethical questions
Dr. Barney Clark, a retired dentist, received a Jarvik-7 artificial heart in 1982 in an effort to save his life. Clark lived for 112 days afterward, but during that time he experienced convulsions, memory lapses, and kidney failure. Retired postal worker William Schroder, the next patient to receive the Jarvik-7 heart, fared better. He lived for 620 days after the operation, but he experienced blood clots and strokes that left him too weak to talk. Subsequently, three other patients who received Jarvik-7 hearts survived for much shorter periods of time. Ethicists began to question whether these procedures improved the patients’ quality of life, or just delayed their death. In 1990, the U.S. Food and Drug Administration withdrew its approval for the Jarvik-7 heart, citing quality control concerns about its manufacturer.

Jeff Topping // Getty Images
2004: First total artificial heart receives FDA approval
The Jarvik-7 artificial heart was renamed the CardioWest Total Artificial Heart after MedForte Research acquired the rights to the Jarvik-7 and formed a partnership with University Medical Center in Tucson, Arizona. In 2004, The U.S. Food and Drug Administration approved the CardioWest TAH as an in-hospital bridge to transplantation, for use in patients who are likely to die within 30 days from biventricular failure. The CardioWest TAH was renamed the SynCardia TAH in 2010. It is still in use today.
BSIP/Universal Images Group via Getty Images
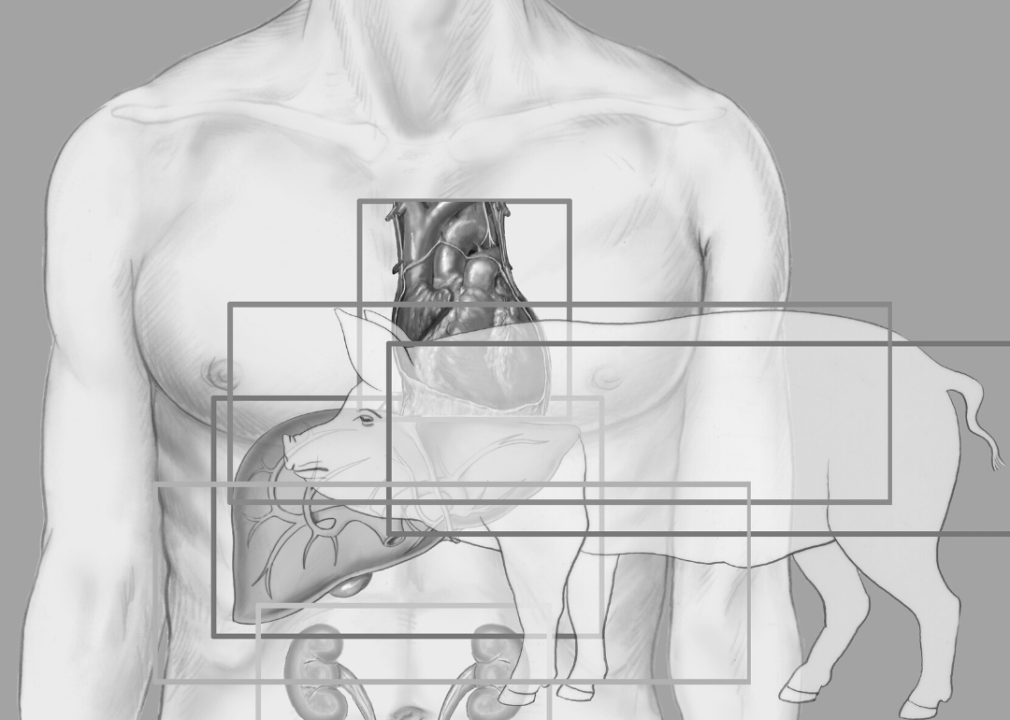
2022: First pig heart transplant
In January 2022, surgeons at the University of Maryland Medical Center transplanted a heart from a genetically modified pig into 57-year-old David Bennett. The organ had 10 genetic modifications to ensure Bennett’s body did not reject the organ, and the modifications also ensured that a heart from a 400 kg animal remained human-sized. The heart functioned well without rejection for about two months, but his condition began deteriorating and he passed away on March 8.
“We have gained invaluable insights learning that the genetically modified pig heart can function well within the human body while the immune system is adequately suppressed,” said Muhammad Mohiuddin, one of the surgeons who performed the procedure. As scientists look ahead, they hope to learn more about the genetic modifications needed in transplanted animal organs and continue clinical trials. Pig-to-human heart transplants are currently limited by the supply of pigs and regulatory hurdles.
This story originally appeared on Healthmatch
and was produced and distributed in partnership with Stacker Studio.