Doctor at Eisenhower Health describes coronavirus ‘hell show’
"Hell show," that's how one doctor at Eisenhower Health in Rancho Mirage describes what's happening there right now with coronavirus.
Dr. Rick Loftus wrote that he wakes up with nightmares every morning, that the situation with coronavirus is getting worse every day, and that people not taking the virus seriously is costing lives.

His lengthy, private communication was posted on Facebook and has gone viral. (You can find Dr. Loftus' full communication at the bottom of the article)
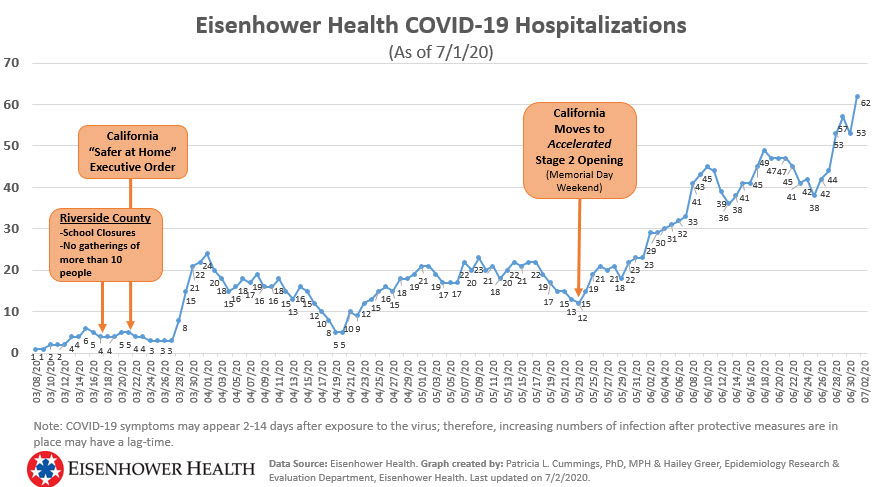
As of July 1, Eisenhower Health reported having 62 coronavirus patients, the highest number of patients since the pandemic started.
Dr. Alan Williamson, Chief Medical Officer at Eisenhower, told News Channel 3 that the hospital is currently at 75 patients today.
Since Eisenhower Health's last update, coronavirus-related hospitalizations across Riverside County continue to increase. Today, the total number of patients surpassed 500 for the first time.
Dr. Williamson joined News Channel 3's Peter Daut during our 6:30 p.m. newscast on CBS & Fox to talk about Dr. Loftus' post and the latest at the hospital.
"We continue to see a steady rise in the number of cases here at the hospital, we're over 75 cases in the hospital today. So just a progressive increase in the volumes, we're still able to keep up with that, but it is continuing to put quite a strain on the healthcare system to be able to meet those demands, to be able to staff the units on a regular basis, this has been going on for over 4 months now, and the staff is getting tired," Dr. Williamson said. "It's hard work, they are having to don the protective equipment and take that off each time they are going in and out of the room with these patients, so physically demanding work as well as mentally taxing and we prepare in healthcare for emergencies that particularly last for days or even weeks at the most, but something that is going to go on for months and months is very taxing for us."
Peter Daut asked Dr. Williamson about Dr. Loftus' report that the Eisenhower Health staff spent time deciding the ethical way to divvy up limited Remdesivir, a drug used to help treat patients with coronavirus.
Dr. Williamson says it's too early for them to make that decision.
"What we are doing is looking at who will be most likely to benefit from the use of Remdesivir," Williamson said. "There is a national shortage of Remdesivir as it is being used rapidly across the country to treat these patients. We are analyzing which patients we believe would best benefit from that, so that when we get to a point where we are running out of that medication, then we can allocate it in a way that makes sense, rather than random allocation, we hope we can identify some patients that are very likely to do extremely well no matter what we do and don't really need to be treated with Remdesivir."
WIlliamson continued, "There maybe some patients we feel the likelihood they're going to benefit and recover if we use that medication is so small, it might not be an appropriate use of that medication. So that's where we are at this point, we're trying to analyze where it makes the most sense to use any precious resource we have. That's not unusual for us to make that kind of analysis."
One of the biggest things that stuck out in Dr. Loftus' post, is that he referred to the hospital as a "hell show."
"I'm glad some of you are sheltered from what unbridled COVID-19 looks like. It's a hell show. This is July. What do you think my hospital will look like in winter," Loftus wrote.
Williamson responded to these claims.
"I'm not even sure what that phrase would mean, we are just doing our job and caring for the patients in the community, it is hard work it is exhausting work for everyone. We do appreciate the support we get from the community who recognize the work we are doing," Williamson said.
WIlliamson says the staff has been tired from all the hard work but everyone maintains a great attitude.
"It is wearing on people because of the duration of this crisis. It is also very heartening when I go out on rounds and go into the COVID units and see the nurses, they continue to have a great attitude, they come into work in the morning, they are wearing to go, they are proud of what they do, they know they are helping the community they're doing what they became nurses to do. And the rest of the support staff as well, not to leave out the respiratory therapists, and nursing aides, and all the other people required to care for these patients. When they go home at the end of the day, I see them dragging out pretty tired. We are concerned about the duration of this event and are we going to start seeing people really just getting worn out and broken down, and potentially getting sick because they are run down. So we continue to do everything we possibly can to rotate staff around, to give them breaks, to be sure that we adjust staffing ratios for it is appropriate for the intensity that's required to care for these patients, but this is a long haul event for us," Williamson said.
Williamson said the hospital is doing okay on capacity right now but they are worried about providing staff in future.
Many of the recent cases have been from younger people but the demographic of cases remains varied which differs from the start of the pandemic.
"We still see 70-, 80-year-olds, but we are seeing some of those 20-, 30-, 40-year-olds, lots of 50-year-olds, so seeing a more broad base demographic across the board rather than an earlier experience which was primarily just the elderly patients," Williamson said.
Nearby Imperial County is also sending patients to Riverside County but not very many.
"We've seen very few patients recently from Imperial County, most of what we're seeing is definitely from our own Coachella Valley area," Williamson said.
Click here to learn more about Imperial County's surge in cases
Williamson also discussed the county's positivity rate. Kim Saruwatari, the county's public health director, said today the county's positivity rate is at 15.9%, almost double the state' threshold of 8%.
"Well positivity rate is an interesting thing, there's so many factors that weigh into that, how many patients are testing, there are continuing to be fluxes from day to day, week to week on who we can test, and how much testing and equipment supplies we can have, so that impacts it, but I don't think there's any question on anyone's mind that there is an upsurge in number of patients as well," Williamson said. "A little hard to reconcile exactly how much of that is some challenges on the testing side, and how much is it true increase on positivity rate across the community, I think it's a mix of both."
Williamson said their current projections show that the pandemic will extend into mid-August.
"Our predictions show that this probably extends to the mid-part of August, and then hopefully we see a peak and then begin to get beyond this, but that means we still have about 6 more weeks that we really need the public to pull out all the stops, do everything we can to try and kill this," Williamson said.
Dr. Loftus' full message:
"I'm in a hotspot hospital in a hotspot region (Coachella Valley, Inland Empire, CA). We just converted the entire second floor of our hospital to COVID-19 care yesterday, July 1. We have 65 inpatients with COVID-19 in a hospital with 368 beds. It is the same at our other 2 hospitals in the Valley. We spent yesterday deciding the ethical way to divide up limited remdesivir (30 patients' worth) for the hospital patients. My 20 incoming interns for our IM resident were exposed to COVID 2 weeks ago during their computer chart training; apparently 100% of our computer trainers had COVID19. One intern tested positive 7 days later and I insisted we re-test them all again, as there are almost certainly other cases with minimal symptoms. I raided my household and took my entire supply of face shields to the hospital for the residents to wear on their first day, and I paid $1000 of my own money to equip all of my residents with medical-grade face shields. I require all residents to wear a surgical mask or N95 with face shield if they are within 6 feet of another human, patient or coworker.
Roughly 20% of our inpatients die. Only 30% of our ventilated patients survive. (We try to avoid ventilation at all costs. Some people insist on being full code and decompensate despite high flow with face mask, proning, dexamethasone, antibiotics, and a cocktail of famotidine, zinc, Vitamin D, Vitamin C, NAC, and melatonin--we throw everything we can at each case, so long as it won't hurt them.)
My administrative assistant, who sits adjacent to the interns, just went home with COVID symptoms. Her test is pending.
In the Southwest, we are experiencing catastrophic exponential growth. I have had multiple families--siblings, parent-child, spouses--admitted with COVID-19. I had a 31 year old come in satting 78% on room air; he had been sequestering himself in his bedroom for a week to avoid infecting his elderly parents, with whom he lived. His sister, the only person he saw outside his immediate household in the 10 days prior to onset of fever, cough, and dyspnea, had also had fevers but had tested "negative" at our other large hospital so he thought it was safe to visit her. (Sigh. The Quest PCR test is about 80% sensitive, we think--it had emergency approval, so sensitivity data was not required. The Cepheid rapid COVID PCR test is 98.5% sensitive but is in short supply due to limited reagent availability.)
I'm glad some of you are sheltered from what unbridled COVID-19 looks like. It's a hell show. This is July. What do you think my hospital will look like in winter?…
This is real. Doctors in places with proper public health responses will see few cases in their hospitals--like UCSF--but let me tell you something: The laws of physics and biology don't change. If you're in an unaffected region, an introduction and poor governance and low use of physical distancing and masks will give you an exponential increase in no time flat (i.e. 2-4 weeks). That's pandemic math. And 20% of the population infected needs a hospital. You will run out of beds with an unbridled pandemic. There is almost ZERO pre-existing immunity to SARS-CoV-2. There may be some "priming" of T-cell responses due to exposure to other "benign" beta-coronaviruses, but we have no idea if that explains the 20-40% of people who seem to get minimal symptoms. Asymptomatic infected persons, however, can, and do, spread COVID to those who die from it.
By the way: I've seen scary looking CT scans of the lungs that look like terrible interstitial pneumonia in a patient who had ZERO symptoms and SaO2 94% on room air. She came in for palpitations and the intern overnight got a chest CT for cardiac reasons. We didn't know it was COVID until her test came back 36 hours later. So "asymptomatic" does NOT mean "no biological activity." The virus replicates furiously in people who feel fine. Kids can spread this as easily as grown ups, even if they feel okay.
Related: I've talked to two previously healthy patients ages 32 and 44 who are 3 and 4 months, respectively, post their acute COVID. They continue to have cough, nightsweats, fever, fatigue. How many survivors have "post-COVID syndrome"? We don't know. Less than 20% but we're not sure. I've asked my hospital to allow me to establish a post-COVID clinic to care for and study survivors. Both NIH and UW are planning similar efforts based on my dialogues with them.
Autopsies show anoxic brain injury in many patients who died of COVID, not to mention microthrombi throughout the lungs and megakaryocytes in massive infiltrations in their hearts and other organs. People get heart failure, lung fibrosis, and permanent kidney injury from COVID-19. This is a disease of the vascular systems, and it can affect any organ, with lungs and kidneys being especially at risk.
In early May, thanks to lockdown, our census of 55 came down to 10 COVID cases, and for a brief moment, I actually had hope that the worst nightmares I had about COVID, as a biohazard virology-trained hospitalist, would not come to pass. Then we re-opened, without test/trace/isolate systems anywhere close to adequate. Eight weeks ago my county decided to make masks "optional," despite 125 doctors begging them not to do that. Now we're worse than we were in April. And it's getting worse every day.
You wanna see if COVID is real? Come walk on my COVID ward with me. It's real. Hearing people talk about it as if it's an exaggeration is, well, rage-inducing, honestly. Denial is the most common reaction to a pandemic. Denial is how the US will wind up with 1.1 million deaths instead of 30,000. I saw AIDS denialists get killed by their belief that HIV "isn't real, it's a pharma conspiracy of the medical industrial complex." Yeah, right, if you say so. I watched patients with those beliefs die.
The hardest part about this is, every new case I treat exposes me. I have assiduous hot zone technique. But no technique is bulletproof. If you keep exposing me to case after case, eventually, the virus will get through my defenses. I'm a 50 year old hypertensive. I don't expect to do well if I get infected. For now, I keep going to work. I'm one of the few pushing forward on COVID clinical trials, basic science, public health messaging, and diagnostic studies at my hospital. I feel a responsibility to keep going. I wake up with nightmares every morning at 4am. But I'm going to keep going for now. I feel very alone a lot of the time. People are not taking this seriously, and it's costing lives. -R
"Everything we do before a pandemic will seem alarmist. Everything we do after a pandemic will seem inadequate. This is the dilemma we face, but it should not stop us from doing what we can to prepare. We need to reach out to everyone with words that inform, but not inflame. We need to encourage everyone to prepare, but not panic." — Michael O. Leavitt, 2007
- Richard A. Loftus, MD
