Older women’s breast cancer is often overdiagnosed, study finds, raising risk of unnecessary treatment
A breast cancer diagnosis is an all-too-common reality for women around the world. In the US
By Amanda Musa, CNN
(CNN) — A breast cancer diagnosis is an all-too-common reality for women around the world. In the US, about 240,000 cases of breast cancer are diagnosed in women every year, the US Centers for Disease Control and Prevention estimates.
Health care providers and patients alike are usually inclined to pursue treatment to stop the disease. But some experts say that it isn’t always necessary to treat breast cancer in older women with aggressive therapy.
A study published Monday in the Annals of Internal Medicine found that large numbers of American women ages 70 to 85 are potentially overdiagnosed with breast cancer and therefore could receive unnecessary treatment.
“Overdiagnosis refers to this phenomenon where we find breast cancers on screening that never would have become clinically apparent,” says Dr. Ilana Richman, the lead author of the study and an assistant professor of medicine at the Yale School of Medicine.
“The breast cancers are real, true cancers under the microscope, but they would have laid dormant in a person’s body and never caused symptoms,” she added. “We wouldn’t have known about that had we not gone looking.”
The study looked at 54,635 women 70 or older who had recently been screened for breast cancer. Richman and her team estimate that 31% of women ages 70 to 74 were potentially overdiagnosed. Among women 75 to 84, an estimated 47% were potentially overdiagnosed.
Women 85 and older were the age group most likely to be overdiagnosed, at 54%.
Breast cancer diagnosis peaks among women in their 70s, according to data from the American Cancer Society. The risk decreases as women age into their 80s, partly “because women die of other health conditions instead like heart disease or other cancers,” Richman says.
Whether an older women should get screened for breast cancer is an individual decision, said Richman, whose study found that overdiagnosis of breast cancer was more prevalent as age increased and life expectancy decreased.
Technological developments drive overdiagnosis
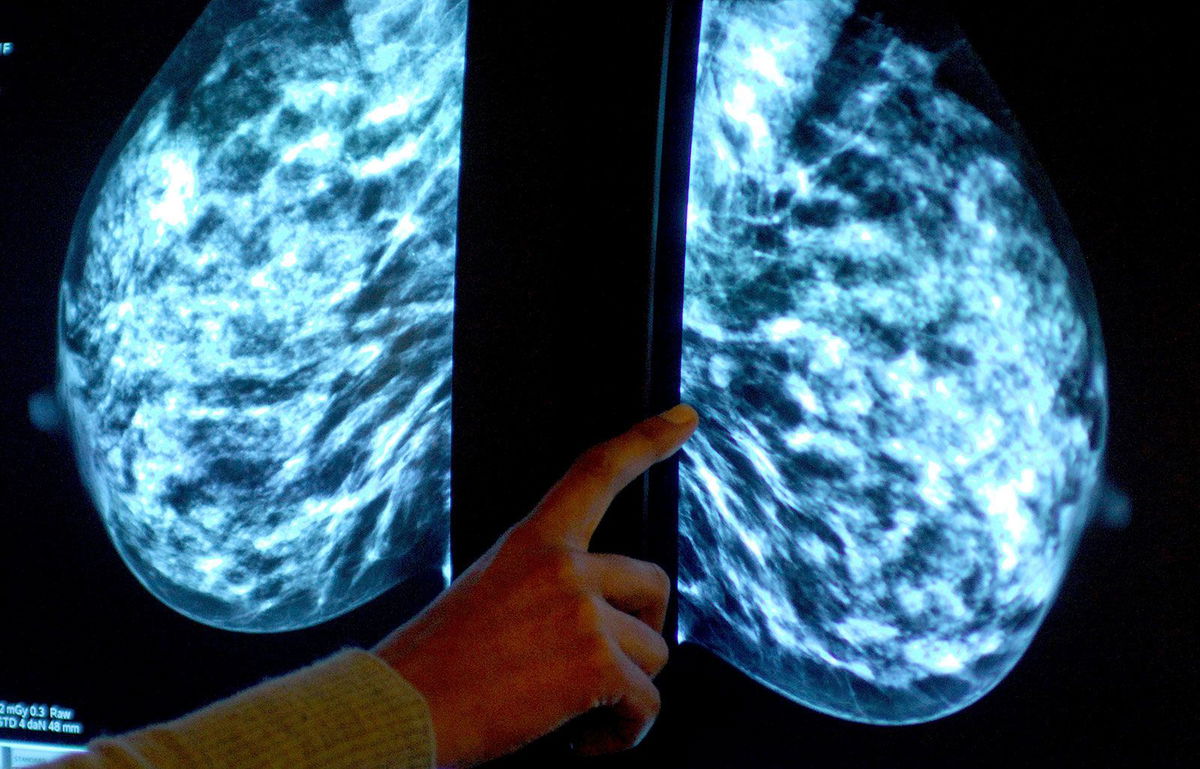
More women are being diagnosed with breast cancer thanks to advancements in screening such as three-dimensional mammography as well as CT, MRI and PET scanning. Technology makes it easier for oncologists to find even the smallest cancer, said Dr. Otis Brawley, an oncologist and epidemiologist at Johns Hopkins University.
“We can now find a lesion in a woman’s breasts that is the size of a green pea,” he said. “We can stick a needle into that woman’s breast and get the needle into that green pea-sized lesion and send a piece of that green pea-sized lesion to a pathologist.”
But Brawley notes that some of these breast cancers are not destined to grow, spread or kill due to their genetic makeup – and meeting them with aggressive treatment such as surgery, radiation or chemotherapy can sometimes be unnecessary and even harmful to the patient.
Not only can overtreatment increase the risk of complications, especially in older patients, it can cause unwarranted stress and financial trouble, he said.
“There’s also the experience of being diagnosed,” Richman says. “It is one of the most life-changing experiences. If we could spare women that experience who don’t need to have it, then I think that would be beneficial.”
She doesn’t want to suggest that less-threatening cancers always go untreated, however. Less-invasive surgery and the use of medications that block estrogen can often treat these cancers sufficiently without exposing patients to radiation or chemotherapy.
Mammograms and older women
For women over the age of 75, there is no guidance on whether to continue getting mammograms, according to the US Preventive Services Task Force, a group of independent medical experts whose recommendations help guide doctors’ decisions. The evidence determining the risks and benefits of screening in women in this age group is “insufficient,” the group says.
In May, the USPSTF issued a draft recommendation urging women to start breast cancer screenings at age 40. It also noted an effort to conduct more research on whether women 75 and older need to be screened for breast cancer.
Mammograms for this age group cost the federal health plan for seniors more than $410 million a year, according to a 2013 study in JAMA Internal Medicine.
Taxpayers usually foot the bill for these tests because most seniors are covered by Medicare.
And while cancer screenings generally aren’t expensive – a mammogram averages about $100 – they can launch a cascade of follow-up tests and treatments that add to the total cost of care.
Much of the screening guidance for mammograms also depends on how much longer a person is expected to live, Richman says, something that’s hard to quantify and a topic that most patients and doctors are not eager to discuss.
“For any one individual in front of you, there’s a fair bit of uncertainty about how long that person will live,” she said. “It also raises issues that are just typical to talk about, like, certainly nobody wants to hear that they’re not going to live long enough to benefit” from a mammogram.
Richman adds that more research needs to be done to conclude whether a woman of a certain age needs to get a mammogram in the first place.
“For women who are getting into the upper age range or women who have lots of other serious medical conditions that are also taking up a lot of time and deserve attention, it’s unlikely that mammography is going to be the thing that is most beneficial to that person’s health.”
Richman also worries about unnecessary exposure to radiation during a mammogram.
Ultimately, she says, the decision to get screened is up to the individual.
“I think for women who are used to being screened and feel like they derive value from knowing something about their bodies, that’s an important consideration,” she says.
The future of breast cancer diagnosis
In the near future, doctors will be able to monitor “good-behaving” breast cancers in the same way low-risk prostate cancers are treated, Brawley said, adding that estimates say “overdiagnosis occurs in more than half of all screen-detected prostate cancer.”
“Within the next 10 years, there will be some women who are going to be told ‘you have breast cancer, but it is one of the more benign breast cancers. Therefore, we’re going to watch you instead of treating you aggressively,” he said.
Ultimately, Brawley says, the answer to overdiagnosis is the study of cancer genomics, analyzing the molecular biology of an individual’s cancer. But the technology is not quite there yet.
“It will lead to a redefinition of cancer. The pathologic definition used today was developed in the mid-19th century using the biopsy and a light microscope. We need to move to a 21st-century definition, encompassing both the biopsy and pathologic appearance as well as genomics,” Brawley says. “The 21st-century definition of cancer will recognize that breast cancer is not one entity but many distinct diseases with potentially different patterns of behavior calling for different treatments and, sometimes, no treatment.”
CNN’s Jacqueline Howard contributed to this report.
Correction: A previous version of this story misspelled Dr. Ilana Richman’s name.
The-CNN-Wire
™ & © 2023 Cable News Network, Inc., a Warner Bros. Discovery Company. All rights reserved.